5 Ways to get through Latching Refusal

Getting to the other side of breast/chestfeeding refusals requires problem-solving from 2 different angles - addressing the underlying causes for the feed refusal (and (and you can check out my last blog on that right here). AND supporting your relationship with feeding and pumping to give yourself the time that is needed to repair what was causing the problem.
In this second part of this blog series, I’m going to talk you through 5 five most important things you can do while you are working on addressing the underlying causes to help make sure you can get to the other side of the refusal and back on track with your feeding relationship.
1. Recognize Your Worry Spiral

When your baby is refusing the breast, it can feel awful. It can feel like the baby is doing more than rejecting your breast, it can feel like they are rejecting you, too
They aren’t. I promise.
They are just telling you that something is hard for them right now.
When we take it to mean our baby is rejecting us, we attach our emotion to whether or not our baby latches, even when we don’t mean to. This causes anxiety around latching and our baby can feel our anxiety, and this makes the refusal worse, and we get into a worry spiral.
A worry spiral happens when we let one worry grow to become something bigger. Our brain morphs “My baby isn’t latching right now” into “my baby isn’t ever going to feed again”, and then we keep going and that turns into a narrative that might look like “I failed my baby” or “I’m a failure as a parent.”
When the truth is that all that happened is that my baby said “I can’t” during a feeding.
A worry spiral doesn’t just impact our emotional wellness. It also impacts our current level of stress. Every time we try to latch our baby we are attaching our stress to that offer. Your body knows, and your baby knows because they can feel it.
Stopping the worry spiral is hard, but it is not impossible. You can do it. It just takes recognizing what is going on, and then working mindfully to change the conversation in your brain.
Remind yourself that whether or not your baby latches in any given feeding isn’t a commentary about your worth or value as a parent or a measurement of love. It's simply a statement about if feeding at your breast/chest is something that they can do right now. At this moment.
Sometimes, changing our language around how we think about latching can help with our perception of what is going on. Instead of saying “He won’t latch”, try “He can’t latch, RIGHT
NOW”. It’s really hard. Trust that if you can get to the bottom of why, then your baby will latch again, and it will be OK.
2. Offer, but don’t force.

We don’t feed better if someone forces us to feed, and your baby doesn’t either. A baby that isn’t latching at your breast/chest isn’t telling you “I won’t”. They are telling you “I can’t”. Whether they have developed a preference for the ease of bottles, or are uncomfortable with feeding, we want to make sure that being in the area where feeding occurs feels safe, even IF feeding isn't happening there.
Make sure you provide lots of opportunities to initiate feeding on their own. This is a great chance to take a bath together, hang out skin-to-skin on your bed, or wear your baby without a shirt on if your environment allows it.
If your baby is already showing signs of aversion - like arching away from you when you offer to feed, then your first step is to go back and establish the safety of being in a feeding place. That means you stop offering altogether until they are no longer instantly wary of being put near your breast/chest. This can take a few days or a few weeks, depending on how significant of an aversion your baby has.
Make sure you give yourself permission for it to take as long as it takes. This is another place you might find that worry spiral popping back up. If you see that creep up on here, give yourself some love, and remind yourself that your baby is biologically wired for feeding. It's not too late, and you aren’t losing time. You are building the foundation of trust that you need.
3. Use Your Night Feedings As an Anchor

Often, babies who are struggling with feeding will feed better at night or during naps than they do when they are awake.
How does this make sense? When your baby is asleep, they are 100% driven by those innate feeding reflexes, because the part of the brain that allows for choice isn’t active. That means the cognitive part of them that has wired “feeding is hard” or “feeding makes my stomach hurt” is also asleep.
That means they are able to feed for longer than they would when they are awake because they don’t have the volitional choice to stop. They stop when they fall back asleep.
Use these feeds.
When babies are having a hard time feeding, they often struggle with getting enough volume while they are awake to maintain their position on their growth curve. Babies often need this night feeding to get the volume they need for growth.
If you feel worried that feeding your baby at night will become a habit or a pattern that you will have to break later, you can put that worry back on the shelf right now.
Remember how we just said that your baby is feeding because they are reflexive, and the part of the brain that uses choice and conditioning isn’t active? How can we condition our brain to do something when the part of the brain that allows for conditioning behavior isn’t active? We can’t.
I can’t will myself to wake up any more than my baby can. I can respond to my environment when I am already awake, however, and when your baby rouses and is feedable, then giving them a chance to feed then helps to protect your relationship for later. You are the one who is conditioned to respond to your baby’s rousing. Not the other way around.
4. Protect your supply in a sustainable way.

Depending on how long your baby has been refusing the breast/chest, and how old your baby is, getting your baby back to feeding at your breast/chest may take several weeks. You need a plan that will help you protect your supply in a sustainable way, to give yourself the time your baby needs to solve their underlying issues.
The key is sustainability, and you have a magic pumping daily pumping number which helps you determine just the right number for you.
If you were to take the number of pumps per day and put them on one side of a graph and the stress level on the other side, There will be a number where your stress level starts to grow. You want to figure out the number of pumping sessions that keeps your stress levels BELOW a 2-3 out of 10. That is your general magic number, and it doesn’t matter what it is.
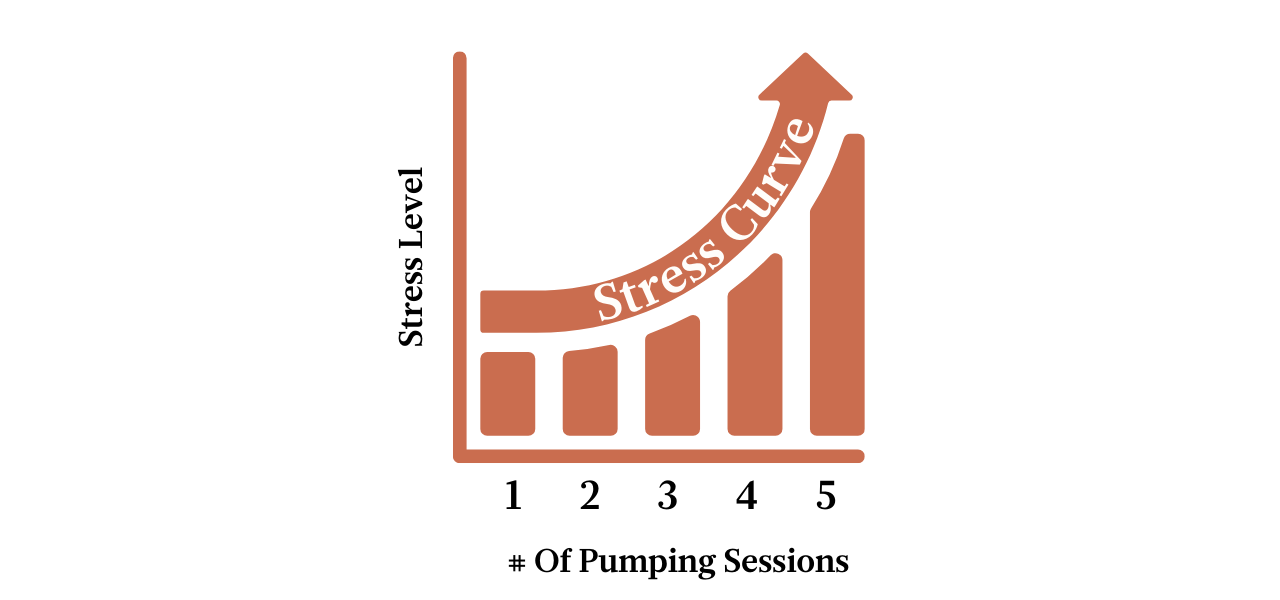
Remember that you will be inclined to overshoot this magic number, and then tell ourself a story about how it will be alright. Your body knows the truth, and it's important to give yourself permission for that number to be whatever it is, without self-judgment or shame.
If your brain defaults immediately to a “but I am going to lose my milk supply if I don’t pump 800 times”, then recognize that worry and put it aside. It's not true. Your milk supply isn’t as fragile as you think, AND stress has a huge impact on your supply. If more pumping causes more stress, then more pumping does not make more milk.
5. Get Good Help

Finding an IBCLC who has a lot of experience in supporting babies through feeding refusals is really important. Figuring out what the underlying cause is can be challenging to do alone. If you are working with an IBCLC you like for latching, ask them what their experience is with feeding difficulties.
Sometimes trying to get to the root of feeding refusals can feel a bit like being a detective, and no one approach works for every baby.
Not all IBCLC’s have the same training and background, and many of us specialize in different things. Some IBCLC’s are really great at supporting and improving supply, some are highly skilled at working at babies with feeding difficulties. You want to make sure you have an IBCLC who is willing to work with you.
Your IBCLC should be able to help you come up with the root cause of your feeding problem, give you a roadmap about how to solve it and provide you with the support you need to help you get to the other side.
If you can’t find someone, let me know. I’m happy to get you pointed in the right direction.



